

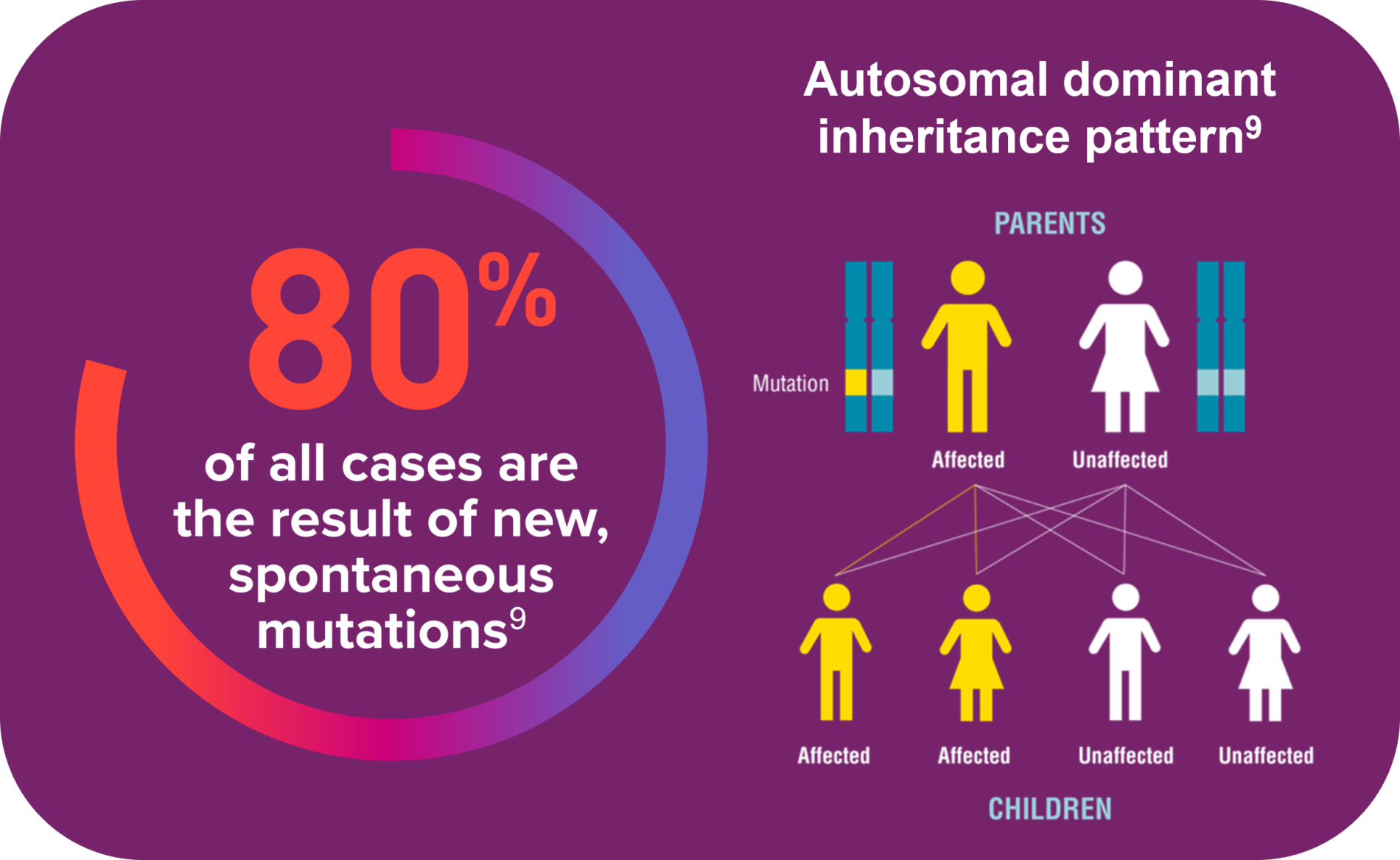
The primary cause is a gain-of-function mutation in the fibroblast growth factor receptor 3 (FGFR3) gene, which inhibits endochondral bone growth7,8
Majority are born to average-statured parents who may not inherently realise the potential lifetime implications of their child’s condition7
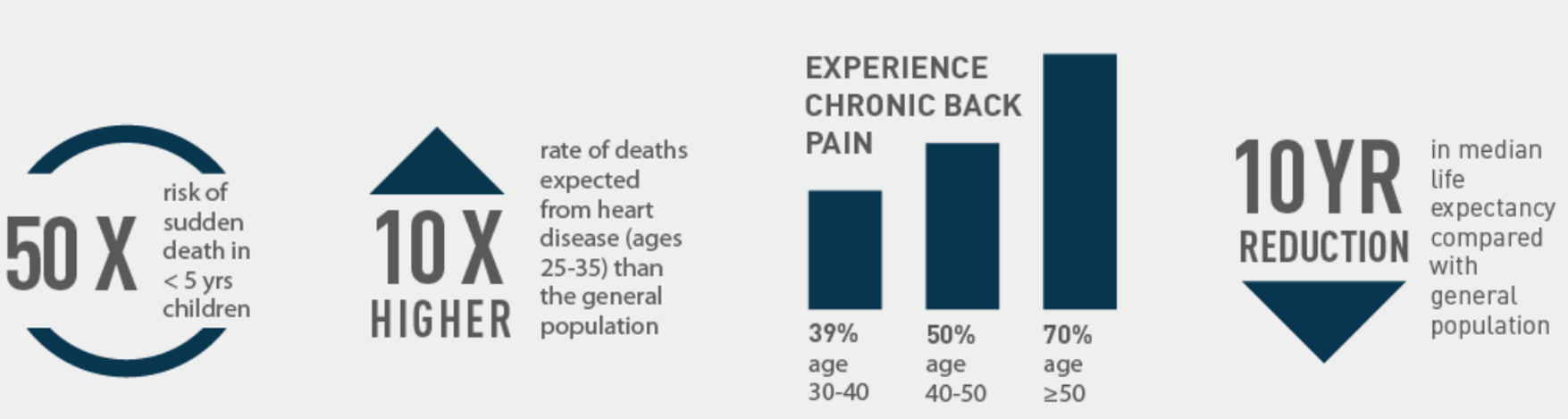
Keep these complications top-of-mind to help give families a holistic picture of what to look out for
Affects >50% of people with achondroplasia
Affects up to 70% of children
Can result in loss of mobility
Can affect walking and running
Misaligned teeth, a narrow palate, open bite, or underbite
Limits their range of motion
Can lead to leg weakness, incontinence, and chronic pain
Limits their range of motion
Can lead to high blood pressure or heart disease
*Potential causes include midfacial hypoplasia & foramen magnum stenosis (a skeletal issue that can result in cervicomedullary compression)